+91 79 26466002, 9099197473
Hepatobiliary surgery
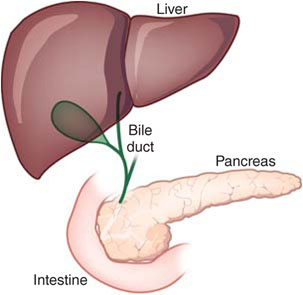
Hepatobiliary surgery is a discipline of gastrosurgery dealing with diseases of liver, bile duct, pancreas and gall bladder.
We provide comprehensive laparoscopic surgery services. The benefits of keyhole surgery have been extended to patients with hepatobiliary diseases. Laparoscopic ultrasonography, laparoscopic cholecystectomy, laparoscopic common bile duct exploration with stone removal, laparoscopic splenectomy, laparoscopic excision of liver cysts and laparoscopic adrenal gland operation are some examples. Special expertise is required in performing laparoscopic cholecystectomy for acute cholecystitis, because it is technically more demanding.
In diagnosis, laparoscopic ultrasonography is a useful assessment tool for patients with hepatocellular carcinoma, and endoscopic ultrasonography for idiopathic pancreatitis. These are some of the highly specialised technology services offered through a multi-disciplinary disease management team in the unit.
Hepatobiliary and pancreatic surgery demands high technical skill. Often, the pathological conditions that affect the liver, gallbladder, bile ducts, pancreas and duodenum are challenging and complex. In general, these conditions can be due to variety of causes such as congenital abnormalities, infection, inflammation, degeneration, benign or malignant tumors, or traumatic injury.
Over the past two decades, hepatobiliary surgery has made tremendous improvement. The high morbidity and mortality rates, once amounted with HPB operations, are now a thing of the past. This is attributed to the better understanding of the liver anatomy, improvement of surgical techniques, better pre-operative imaging, advances in anaesthesiology and surgical intensive care. Liver and pancreatic operations have become safer and less morbid with a low death rate and high success rate.
We endeavour to continually improve our management of hepatobiliary and pancreatic conditions by mastering advanced procedures & complex surgery that will prolong our patient’s survival and improve their quality of life.
Service
Liver
- Liver tumours
- Liver cancers
- Liver cysts
- Liver metastasis
- Liver Infection and Abscess
- Echinococcosis / Parasite Infestation
- Liver trauma
- Portal Hypertension and Liver Cirrhosis
- Segment-oriented Anatomic Liver Resection Surgery
- Three Dimentional Reformatted Images Operation Planning
- Chemoembolization of Tumors Liver
- Radiofrequency Induced Thermal Ablation of Liver Tumour
GALLBLADDER
- Cholecystitis (gallbladder inflammation) / Gallbladder infection
- Cholecystolithiasis (gallbladder stones)
- Congenital deformities: choledochal cysts and etc
- Gallbladder cancer
- Gallbladder polyps
- Cholesterosis
BILIARY TRACT
- Biliary Tract Stricture (narrowing)
- Acute Biliary Tract Infection: Cholangitis
- Endoscopic, Laparoscopic and Endo-laparoscopic Surgery
- Recurrent Pyogenic Cholangitis
- Primary or Secondary Choledocholithiasis (common bile duct stones)
- Biliary Tract Cancer: Peripheral, Hilar and Distal Duct Cholangocarcinoma
- Biliary Reconstruction for Stricture or Cancer (operation to re-establish bile flow into the small intestine to provide drainage without reflux)
PANCREAS AND SPLEEN
- Pancreatic Cancer
- Pancreatic Cyst and Cystic Tumours
- Chronic Pancreatitis
- Pancreatic Endocrine Tumours
- Acute Pancreatitis
- Congenital Anomaly
- Pancreatic Traumatic Injury
- Whipple’s Operation: Pylorus Preserving and Conventional
LIVER & PANCREATIC RESECTION TECHNIQUE & TECHNOLOGY
- Technique:
- Segment-oriented Anatomic Liver Resection Surgery
- Parenchyma Sparing Liver Resection
- Extra-Glissonian Extra hepatic Inflow and Outflow Control
- Surgical Stapler Assisted Liver Parenchyma Resection
- Pancreas
- Duodenal Preserving Pancreas Resection Surgery
- Spleen Preserving Distal Resection Surgery
- Segmental Pancreatic Resection
- Pancreas Preserving Duodenectomy
- Transduodenal Ampullectomy
Treatment Options for Liver Cancer
Major liver resections are now routinely performed for liver cancer. Surgery offers the chance for long-term survival for liver cancer patient. Liver tumors that cannot be removed for various reasons can be destroyed with alternative methods such as radiofrequency ablation technique or alcohol injections into the tumor. Other effective modalities include chemotherapy with embolization of the vessels nourishing the tumor, or through a hepatic artery pump.
1. LIVER RESECTION SURGERY
Liver can be resected up to 75% of its volume. After liver resection surgery, the remaining liver can regenerate to its original size in about two weeks. The operation is performed to remove the liver tumours with the goal of completely removing the portion of the liver where the tumour is located and normal liver tissue is preserved as much as possible. This is achieved by parenchyma preserving segment oriented anatomic liver resection. This technique is particularly important for patients with compromised liver function from the underlying liver disease such as liver cirrhosis.
2. TRANSARTERIAL CHEMOEMBOLIZATION (TACE)
TACE is a treatment option for patients with liver cancer. A small catheter is inserted in an artery through the groin. Under the guidance of an X-ray, the catheter is threaded into the artery that provides blood into the liver as well as the liver tumor. Then a high concentration of chemotherapy is injected directly into the tumor. In addition to the chemotherapy, the blood supply to the tumor is blocked (embolized) by injecting some particles. Over time, this treatment causes the tumor to decrease in size or break down completely.
3. RADIOFREQUENCY ABLATION (RFA)
RFA is used to treat tumors that cannot be surgically removed because of the tumor size or location. RFA is a process in which radiofrequency energy is delivered to the liver tumor to destroy the liver tumor. Ultrasound is used to precisely target the liver tumor using an electrode needle system. This radiofrequency energy produces heat that destroys the tumor without causing much harm to the surrounding healthy liver tissue.
4. PERCUTANEOUS ETHANOL INJECTION THERAPY (PEIT)
PEIT is used to treat liver cancer that may be difficult or unsafe to ablate with thermal radiofrequency. The alcohol injected into liver tumor causes the tumor to dry out and eventually break down. Ultrasound is used to guide the injection of alcohol through the skin via the liver into the liver tumor. Ethanol injection is effective in treating patients with small liver cancer.
Treatment plan for pancreatic disease
1. PANCREATIC TUMOR
The most frequent malignant tumor of the pancreas is the ductal- adenocarcinoma, usually located in the head of the pancreas. We have favoured Pylorus Preserving Pancreaticoduodenectomy (PPPD) over the conventional Whipple’s. In PPPD, the stomach is preserved whilst in the conventional operation, one third of the stomach is removed. Studies have found that PPPD does not compromise the oncological resection, but by preserving the gastric function, the patient’s quality of life can be improved. We have also developed strict protocol and care-paths on how to manage such patients before their operation, during the operation and after the operation.
2. CYSTIC TUMORS AND OTHER LESS AGGRESSIVE TUMORS OF THE PANCREAS
With a multi-disciplinary pancreatic management team, we work closely with our gastroenterologist, which allow the surgeon rapid access to Endoscopic Ultrasonography for characterization of pancreatic lesions. This information is extremely useful in the management algorithm. For selected patients with optic tumors and other less aggressive tumors, we can contemplate more tailor-made parenchyma preserving procedures such as segmental pancreatectomy and spleen-preserving distal pancreatectomy.
3. CHRONIC PANCREATITIS
Many patients with this disease suffer from chronic pain, which may be debilitatory. In our multi-disciplinary team, we have inputs from our pain specialists, as well as our endocrinologists, who will address the endocrine insufficiencies. If despite pharmacological agents, the pain remains an issue, we have other modalities like coeliac neurolysis, or even thoracoscopic sympathectomy. If patient has an inflammatory pancreatic head mass, we can also perform a duodenum-preserving pancreatic head resection: either a Beger procedure or a Frey’s procedure or a Berne modification of the Beger procedure.